AMT Endoscopy in Singapore: Expert Care.
Now, over 40% of advanced endoscopic devices in Southeast Asia have precision parts from Metal Injection Molding. This boosts safe, speedy procedures across the area.
Let’s talk about how AMT in Singapore is leading with their blend of clinical skills and high-tech manufacturing for endoscopy. Their approach combines MIM, 100K cleanroom assembly, and ETO sterilization. This enables single-use devices and sterile, peel-open packaging for endoscopy by AMT.
Endoscopy centers in Singapore are seeing significant benefits. Improved imaging, miniaturized optics, and strong training programs lead the way. For patients, that means minimally invasive diagnostics and therapies, shorter sedation times, and faster recovery.
AMT’s contributions also address broader challenges such as cost pressures, specialist availability, and regulatory compliance region-wide. This article outlines how AMT’s endoscopy capabilities support clinicians and patients alike. Focus areas include access, safety, and cost reduction.
Essential Conclusions
- Endoscopy by AMT combines MIM manufacturing with cleanroom assembly and ETO sterilization for reliable components.
- AMT-enabled devices support HD, minimally invasive procedures that improve patient recovery.
- Singapore endoscopy centers leverage AMT’s parts to strengthen clinical workflows and device safety.
- Advanced devices reduce sedation and enable diagnostic-plus-therapeutic procedures in one session.
- Access is shaped by cost, specialist training, and regulatory requirements across the region.
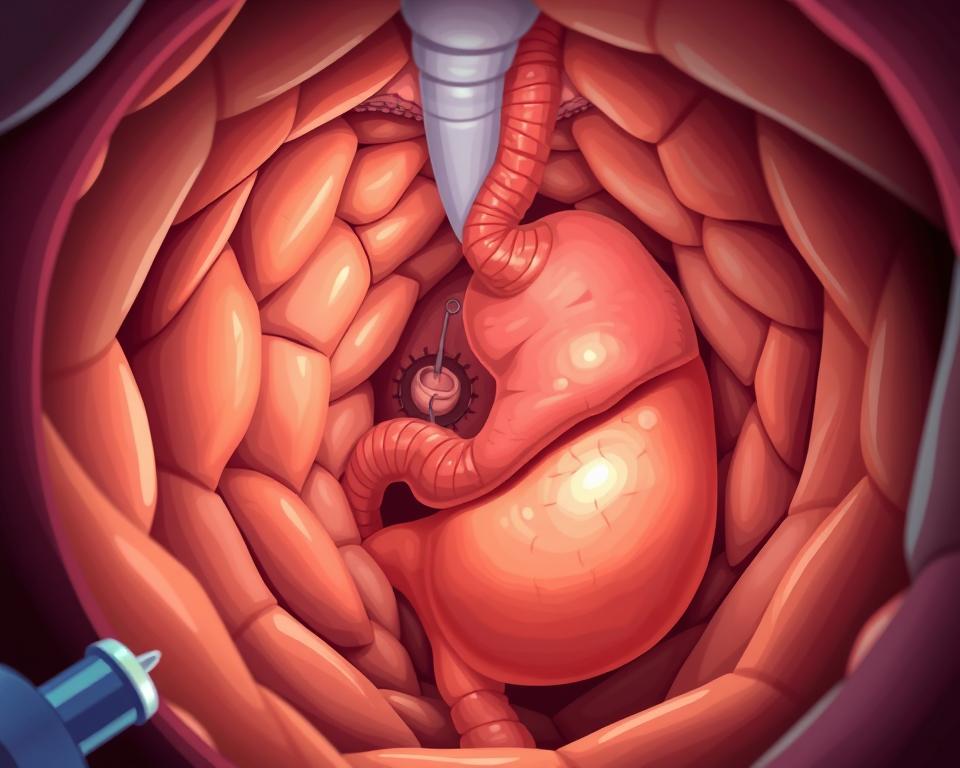
Endoscopy Explained and AMT’s Contribution
Endoscopy is a way doctors can look inside the body without big cuts. They use tiny cameras on flexible or rigid scopes. This method lets doctors see, diagnose, and treat problems in one go. It cuts down on recovery time and avoids big surgeries.
Definition and purpose of endoscopy
Doctors use endoscopy to check out areas like the stomach, lungs, and kidneys. They can take samples, remove growths, and do treatments with little cuts. Patients often need less sedation, leave sooner, and return to normal activity faster.
AMT’s Tech-Driven Endoscopy Support
AMT makes special parts that help endoscopes work better. Using MIM and cleanroom assembly meets stringent standards. Components such as biopsy tools and electrodes arrive sterile and ready to use. This supports faster workflows and safer patient care.
From Early Scopes to HD Miniaturization
Early endoscopes of the 19th century were basic tubular devices. Today’s systems use mini digital cameras and highly flexible scopes. Better cameras and lights help doctors see clearer and diagnose better. Early-stage AI assists with faster lesion detection.
Thanks to companies like AMT, these tools are getting even better. Clinicians in Singapore perform more complex therapy with reduced risk. This means patients get top-notch care without big surgeries.
AMT Endoscopy Solutions
AMT is your all-in-one partner for those making devices and hospitals in Singapore. They blend fine manufacturing, cleanroom assembly, and sterilization for use-ready tools that match clinical timelines. This method speeds up device development from quick prototyping to full-scale production, all while focusing on regulatory requirements.
What AMT Delivers for Endoscopy
AMT provides MIM, precision component sourcing, 100K cleanroom assembly, and ETO sterilization. The company aids in producing single-use devices, sterile packaging that peels open, and sterilization after manufacturing so instruments can go straight to the operating room. This results in shorter waiting times for manufacturers and gives doctors sterile, ready-to-use tools right away.
How AMT integrates manufacturing (MIM) and device design
MIM allows for the creation of complex shapes and tiny features tough to make by other means. AMT combines MIM with design focused on manufacturing to cut down on the number of parts by merging several into one. Results include tight precision at micro-scales, improved reliability, and reduced assembly time.
AMT Component Examples for Endoscopy
AMT supplies biopsy forceps and graspers for GI/urology, clamps and scissors for delicate handling, and precision biopsy needles. They also offer single-use TURP bipolar electrodes in stainless steel or tungsten alloy, all sterile in packages that peel open. Each item is built with consistent quality and assembled under clean conditions for clinical safety.
| Component | Manufacturing Method | Typical Materials | Clinical Use |
|---|---|---|---|
| Biopsy forceps (GI/Uro) | MIM with secondary finishing | 316L stainless steel | Tissue sampling in GI and urology |
| Endoscopic graspers | MIM precision forming | Stainless steel, tungsten alloys | Tissue handling and retrieval |
| Bipolar TURP electrodes | MIM with post-machining | Tungsten alloy, stainless steel | Bipolar resection (urology) |
| Clamps and micro-scissors | MIM + micro-machining | Medical-grade stainless | MI instrument tips |
| Precision biopsy needles | MIM + heat treatment | Stainless steel | Targeted tissue extraction with precise geometry |
With AMT’s endoscopy solutions, the number of assembly steps drops and consistency in each batch goes up. Clinicians receive sterile, packaged, ready-for-surgery devices. Manufacturers achieve efficient, cost-effective scaling.
Singapore’s Advanced Endoscopy
Singapore offers a broad spectrum of advanced endoscopy methods. These are for diagnosis and treatment. Top hospitals and centers run advanced endoscopy suites. They deploy the latest tools for simple and complex cases alike.
GI Capabilities in Endoscopy
Gastrointestinal endoscopy includes procedures like esophagogastroduodenoscopy and colonoscopy. They offer direct viewing, targeted biopsy, polypectomy, and control of bleeding in one session. Techniques like endoscopic mucosal resection and submucosal dissection can treat early cancers. All without open surgery.
Minimally Invasive Approaches & Recovery
Minimally invasive endoscopy uses flexible scopes, tiny cameras, and tools for treatment. These advances lessen tissue damage and reduce the need for sedation. Thus, patients usually have shorter hospital stays. Patients resume normal activities sooner and face fewer complications than with open surgery.
Therapeutic endoscopy that combines diagnosis and treatment in one procedure
Many procedures combine diagnosis and therapy in one sitting. Physicians can identify and remove polyps, biopsy tissue, and perform coagulation/resection simultaneously. It reduces the need for multiple anesthesia doses, cuts down on hospital times, and enables care in outpatient or day surgery settings.
Advanced endoscopy in Singapore is enhanced by AMT-enabled tools and precise components. Innovations support higher accuracy and safer complex procedures. Consequently, regional patients access more up-to-date care.
Endoscopy technology and instrumentation from AMT
AMT delivers clinical-grade innovations for endoscopy. They bring together optics, precise metals, and disposable items. This helps doctors see clearer and work safer during procedures.
High-definition imaging, miniaturized cameras, and lighting systems
Surgeons receive crisp, real-time imagery via HD and mini cameras. Bright LEDs and fiberoptic lights boost color and detail. This accelerates detection and supports shorter, safer procedures.
How MIM Enables Precision Parts
MIM lets AMT make precise metal parts for endoscopy. Biopsy forceps, grasper jaws, and electrode tips are made durable and fit well. Part consolidation reduces assembly steps and boosts reliability.
Single-use instruments and sterile packaging practices for safety
Single-use tools arrive sterile to lower infection risk. ETO sterilization and clean assembly underpin safety. Sterile-barrier packaging and lot traceability secure workflows.
| Feature | Clinical Benefit | AMT capability |
|---|---|---|
| HD imaging | Improved lesion detection and treatment precision | Integrated CMOS cameras with LED/fiber lighting |
| MIM precision parts | Precision, strength, and consolidation | MIM for forceps, electrodes, micro-instruments |
| Single-use endoscopes & instruments | Lower infection risk, simpler reprocessing | Sterile-peel packs, ETO sterilization, cleanroom assembly |
| Traceability & packaging | Regulatory compliance and supply chain confidence | Lot traceability, sterile barrier systems, validated processes |
AMT unites imaging, MIM components, and single-use tools for modern practice needs. They focus on accuracy, reliability, and safety in Singapore and beyond.
Endoscopy services and patient care in Singapore
In Singapore, hospitals and special clinics have a strong network for endoscopy services. Expert teams, including gastroenterologists and endoscopy nurses, use top-notch equipment to manage patient care efficiently. High-quality devices support safety for local and international patients.
How AMT components support clinical workflows
AMT’s precision parts for endoscopy help avoid equipment failures and keep schedules on track. Exacting instruments (e.g., biopsy forceps) speed case turnover. Reliable quality smooths procedures and reduces delays.
Improved Patient Experience
Modern equipment with thinner scopes increases patient comfort. Many patients need only light sedation due to these advances. The result? Less harm to tissue and quicker home returns.
Sterilization and cleanroom integration
AMT aligns with Singapore’s hospital sterilization methods, using cleanrooms and ETO sterilization. Single-use options reduce reprocessing workload and infection risk. This approach ensures equipment is safe and ready for patients.
Operational efficiencies and service ecosystem
Disposables accelerate turnover and free staff for clinical tasks. Consistent AMT supply keeps high-demand services running smoothly. This teamwork makes sure every patient gets consistent, high-quality care.
| Operational Need | AMT Contribution | Benefit for Patient Care |
|---|---|---|
| Instrument reliability | Precision MIM components for forceps and graspers | Fewer procedure delays and safer outcomes |
| Turnover time | Single-use devices, stocked sterile kits | Faster patient throughput and reduced wait times |
| Sterility assurance | 100K cleanroom + ETO | Lower infection risk, compliant flow |
| Patient comfort | Mini scopes, refined accessories | Less sedation, less discomfort, quicker recovery |
Endoscopy specialist skills and training
To work with modern endoscopy tools, you need both education and hands-on experience. GI, urology, and surgical specialists complete focused training. They also practice a lot with simulations and real procedures. This way, they learn to safely use the latest technology.
Operating Advanced Endoscopy Systems
Training for endoscopy focuses a lot on doing many procedures and checking skills. Trainees practice with HD imaging, energy devices, and system management. Education covers component selection and safe disposable use. This reduces equipment-related errors. Formal assessments and proctored cases are common.
Expertise Concentration & Access
In Singapore, advanced training concentrates in major hospitals. These places become experts because they handle many cases. But, people living far away might find it hard to get to these specialists. Health systems have to think about whether to spread out resources or keep them centralized.
Ongoing Education & Competency
Teams must keep pace with new tools and computer-aided imaging. They often check their work and learn from mistakes to stay safe. Vendors such as AMT offer courses to deepen technical understanding. Up-to-date training means fewer issues and higher patient satisfaction.
Workforce & Cost
Keeping a team skilled involves spending on training and time for teaching. These costs influence treatment pricing. Planning how to grow the workforce ensures that more people can get advanced endoscopy as needed.
Endoscopic procedures covered and clinical indications
Endoscopic procedures cover a broad scope of both checking and fixing health issues. In Singapore, clinicians apply these methods widely. They check symptoms, handle benign (non-cancerous) problems, and take tissue samples with little trouble for the patient.
Common gastrointestinal procedures
Upper endoscopy and colonoscopy identify bleeding, investigate dyspepsia, and support colorectal cancer screening. Therapeutic tasks include polypectomy, resection, hemostasis, and targeted biopsy. AMT-supplied tools enable precise sampling for early cancer detection.
Urology Use Cases
Ureteroscopy and cystoscopy let doctors see directly inside the urinary tract to find stones, blockages, and tumors. A common procedure for enlarged prostate is transurethral resection. TURP electrodes are precisely manufactured. Tips use stainless or tungsten alloys for resection and coagulation.
When minimally invasive endoscopy is preferred
MI endoscopy is preferred for early tumors, benign obstruction, and urgent bleeding. It’s also favored when less invasive sampling is safer than open surgery. People with other health problems also get better faster and need less time under anesthesia with this method.
Decision Factors
Choosing between endoscopic procedures and open surgery depends on the health issue, size and location of the lesion. The choice also relies on the available skills and tools. Patient preference and expected recovery time are important considerations.
| Indication | Common Endoscopic Approach | AMT Component Role |
|---|---|---|
| UGI bleeding | UGI endoscopy + hemostasis | HD optics + forceps for targeted sampling/coagulation |
| Polyp (colorectal) | Colonoscopy with polypectomy or EMR | Mini graspers/snares via precise MIM |
| Suspected bladder tumor | Directed biopsy via cystoscopy | Durable single-use biopsy instruments and endoscopic cameras |
| Benign prostatic hyperplasia (BPH) | Transurethral resection using bipolar energy | TURP electrodes with single-use stainless steel or tungsten alloy tips for resection and coagulation |
| Stone (ureteral) | Ureteroscopy with laser lithotripsy | Precision tips and mini shafts for passage and manipulation |
Regulatory and Sterility Considerations
Patient safety relies on careful cleaning, assembly, sterilization, and record-keeping. AMT uses advanced 100K cleanroom assembly lines. These lines combine top-notch assembly methods with reliable sterilization processes. This improves infection prevention and meets hospital standards.
AMT Clean Assembly process concludes with sterile, ready-to-use devices. For reusable tools, AMT provides validated cleaning/sterilization guidance. They also explain which sterilization methods work best. ETO is key for heat-sensitive items, ensuring safety and audit readiness.
When choosing between single-use or reusable instruments, it’s important to consider several factors. Single-use reduces infection risk and simplifies compliance. On the other hand, reusable devices can save money but require a strong system for cleaning and sterilization to stay safe.
In Singapore, medical devices must meet certain standards. Firms register with the HSA and adhere to ISO 13485. Their electronic parts need to meet certain IEC standards. Also, providing clinical evidence and conducting post-market surveillance are crucial for keeping up with regulations.
Medical tourism brings extra challenges. Hospitals serving international patients maintain detailed device provenance, sterilization history, and staff training records. Such documentation is necessary to meet the standards of foreign insurance and accreditation organizations. It supports informed choices and a sterile, traceable supply chain.
| Aspect | Single-use | Reusable |
|---|---|---|
| Cross-infection risk | Low; one-and-done use lowers cross-contamination | Depends on validated reprocessing + tracking |
| Cost profile | Higher consumable cost per case; lower capital outlay | Higher upfront capital; lower per-case consumables over time |
| Sterilization | ETO-sterilized or aseptically packaged, delivered sterile | Requires autoclave, ETO sterilization, or validated cycles per material |
| Regulatory & documentation | Simpler traceability for single lots; packaged sterile barrier records | Comprehensive reprocessing logs, maintenance, and performance validation |
| Environmental impact | More waste volume; recycling programs emerging | Lower disposable waste; energy and water use in reprocessing |
| Operations | Reduces reprocessing workload; faster turnover between cases | Needs staff, validated SOPs, and processing downtime |
Hospitals should weigh risk, cost, and compliance when selecting solutions. Good recordkeeping, proper ETO sterilization processes, and clean assembly are crucial. They ensure safety in endoscopic care and help meet regulatory standards.
Economic and access considerations for advanced endoscopy in Singapore
Advanced endoscopy has clear benefits for patients. High-definition equipment and special tools make costs go up. These costs affect how much hospitals charge for procedures and how providers set up their services.
Endoscopy suites with the latest tech can be very expensive. Ongoing maintenance adds yearly operating expense. The use of disposables and the need for ongoing training also make things pricier. All these factors contribute to the overall cost of endoscopy services for patients and healthcare facilities.
Medical tourism and regional demand
Hospitals in Singapore attract patients from across Southeast Asia. Patients seek complex procedures unavailable locally. Shorter wait times and high-quality service are big draws. Partnerships help keep costs down and service consistent for visitors.
Lifecycle Cost Considerations
Hospitals balance upfront and lifecycle costs. Frequent need for disposables and new parts can add up. Smart contracting and inventory control can reduce strain. Transparent accounting enables fair center-to-center comparisons.
Equity and two-tier access risks
Focusing advanced care in select centers can make healthcare gaps bigger. Access hinges on funding and insurance. If unmanaged, benefits skew to wealthier patients. Planning should aim for equitable distribution.
Policy levers and collaboration
Working together, the public and private sectors can make care both innovative and affordable. Subsidies and transparent pricing ease pressure. Safe disposable strategies can reduce infection risk without undue cost. These efforts help more people get the care they need fairly.
| Factor | Impact on Pricing | Potential Policy Response |
|---|---|---|
| Capital equipment | Large upfront cost raises per-procedure amortization | Subsidies, leasing, shared public suites |
| Maintenance/software | Annual contracts add predictable OPEX | Competitive bidding, multi-year service agreements |
| Disposable consumables and single-use devices | Direct per-procedure cost increases | Evidence-based use, reimbursement tuning |
| Specialist training and staffing | Higher labor and credentialing costs | Government-funded training, regional skill centers |
| Tourism demand | Revenue can help subsidize advanced services | Quality accreditation, transparent pricing for international patients |
| Supply-chain integration (manufacturing, sterilization) | Better availability can lower AMT endoscopy cost | Local incentives, AMT partnerships |
| Insurance and subsidy models | Determines patient out-of-pocket burden | Expanded coverage for priority procedures, means-tested subsidies |
Future trends: AI, telehealth integration, and manufacturing advances
Innovation is changing the way endoscopic care is given in Singapore and nearby areas. New technologies in imaging, connecting remotely, and making things are coming together. The result: expanded capabilities, easier workflows, and lower per-procedure cost. These changes affect doctors, companies making devices, and hospitals.
AI for Detection and Triage
Machine learning now helps doctors spot small lesions and figure out what kind of polyps are there during checks. AI support improves accuracy and reduces misses. It acts like an extra set of eyes during procedures.
Using AI in endoscopy needs careful checking, clear metrics for performance, and rules to stop bias in algorithms. Clinical teams must learn to interpret AI outputs and balance them with clinical judgment.
Remote Support & Tele-Endoscopy
Telehealth enables remote oversight and consultation. Experts from afar can watch procedures live, help decide on biopsies, and give second opinions from different places.
Remote device management reduces in-person adjustments and PPE use. Teams monitor health, schedule maintenance, and update systems proactively.
Manufacturing for Scalable Precision
MIM lowers the cost of producing small, precise parts for modern scopes/tools. MIM consolidates steps, cuts assembly time, and scales output while maintaining quality.
Faster prototyping and lower unit cost support rapid iteration. Consistency increases device longevity and supports steady clinical supply.
Practical Implications
AI, telehealth, and MIM improvements enable distributed care and faster diagnosis. Health systems should update training, invest in cybersecurity, and clarify data governance.
Companies that make endoscopy devices should work with doctors. They need to check how things work and fit AI support and remote management smoothly into daily uses.
| Trend | Key Benefit | Primary Challenge |
|---|---|---|
| AI-assisted detection | Better detection and standardized interpretation | Validation & bias control, governance |
| Tele-endoscopy | Remote expertise and centralized oversight | Bandwidth, privacy, workflow integration |
| MIM manufacturing | Scalable, precise components with lower unit costs | Tooling, QC, and traceability requirements |
| amt endoscopy solutions | End-to-end continuity of device supply | Interoperability, training, maintenance models |
The Final Word
AMT’s endoscopy in Singapore uses precise manufacturing and cleanroom assembly. This supports high-quality, minimally invasive care. Solutions include clear imaging, dependable single-use tools, and durable components.
The perks include better diagnosis with HD images and AI. Procedural workflows are more streamlined. This means big improvements for endoscopy departments.
However, challenges include equipment and training costs. Strict regulatory compliance is also required. Choosing between reusable and disposable tools impacts infection control and costs. Addressing these ensures broader, equitable access.
In the future, blending AI, telehealth, and better manufacturing will enhance endoscopy services. In Singapore, manufacturers, providers, and policymakers must collaborate. Their goal? To make sure endoscopy help is safe, affordable, and available to all.